This is my free weekly newsletter covering 5 interesting points from the week. Subscribe (if you haven’t already) if you’d like to get it in your inbox each week!
1. Hypnosis grows breasts? 🤨(Two papers)
A 1974 study describes an experiment done on 19 women aged 18-40 years old. First, a control group of three women were hypnotized once weekly. In the experimental group, three women were hypnotized once weekly and given hypnotic suggestions for breast growth. The hypnosis sessions averaged from one to two hours each, and were continued for a period of twelve weeks.
The control group experienced no change in breast size, but all three of the women in the experimental group experienced an increase in breast measurements.
In the second phase, each of the remaining thirteen subjects received weekly hypnosis during and suggestions were given for breast enlargement. All of the women experienced an increase in breast measurements following treatment, with an average increase of 2.125 inches.
The authors remarked that “Further investigation may show this procedure to be a satisfactory alternate method to surgical breast augmentation.” Surely no one would waste their time investigating this any further… right?
A study titled Hypnotic Stimulation of Breast Growth was published in 1977. Another group from the University of Houston wanted to see if the previous study’s results could be replicated. Three adult women were hypnotized and given hypnotic breast-increasing suggestions. The three women all experienced an increase in breast size. The average breast size increase was similar to the previous study - about 2 inches.
They followed up with the women 3 months later and found that they had retained 81% of the breast size increase.
I have no further comments.
2. Is light better than vegetables?
One of the key selling points of vegetables is that they provide antioxidants. For example the popular Bryan Johnson adds plenty of broccoli to his longevity-boosting “super veggie” meal - a meal where “every calorie has to fight for its life.” Broccoli makes the cut for him because it has antioxidants and fiber.
Long story short, the free radical theory of aging states that oxidative damage in the body accumulates over time, affecting cellular components like DNA, proteins, and lipids, which in turn contributes to the aging process. So antioxidants would theoretically mitigate some of this damage.
Bryan Johnson also wisely invests some time into red light therapy or “photobiomodulation.” A 2016 study found that photobiomodulation increases levels of one of the body’s most potent natural antioxidants, glutathione. Photobiomodulation (PBM) just means “modulating biology with light” - it’s also referred to as “light therapy,” usually “red light therapy” because as in the case of this study, around 660nm light is used.
As you can see, the injured (CCI) rats had their glutathione dramatically reduced in response to the injury, but the red light therapy raised it enough to get back to baseline.
Various rodent studies have noted the antioxidant properties of PBM.
Another study found that PBM therapy has an antioxidant effect in the lungs of male rats exposed to formaldehyde. Another study in diabetic rats found that photobiomodulation (PBM) may be able to improve function of diabetic stem cells and increases gene expression of antioxidant agents.Another study in rats found it to reduce brain inflammation and oxidative stress. Another study in mice found 660nm light to reduce oxidative stress and increases BDNF levels in the hippocampus.
A study on the promise of photobiomodulation for traumatic brain injury explains:
PBM generally produces ROS at low levels, resulting in positive effects [28]. PBM has been shown to modulate ROS levels positively, increasing antioxidant enzyme activity in superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GPx), leading to the reduction of oxidative stress in brain tissues [29,30]. Injured cells subjected to high levels of oxidative stress, such as in the case of TBI, are also more responsive to PBM. It has been found that the more stressed the cells are, the better they respond to PBM [31]. The response tends to decrease the intracellular concentration of ROS [32].
That is, photobiomodulation stimulates the body to produce more of its natural antioxidants (which reduces oxidative stress in the brain). These include glutathione, superoxide dismutase and catalase.
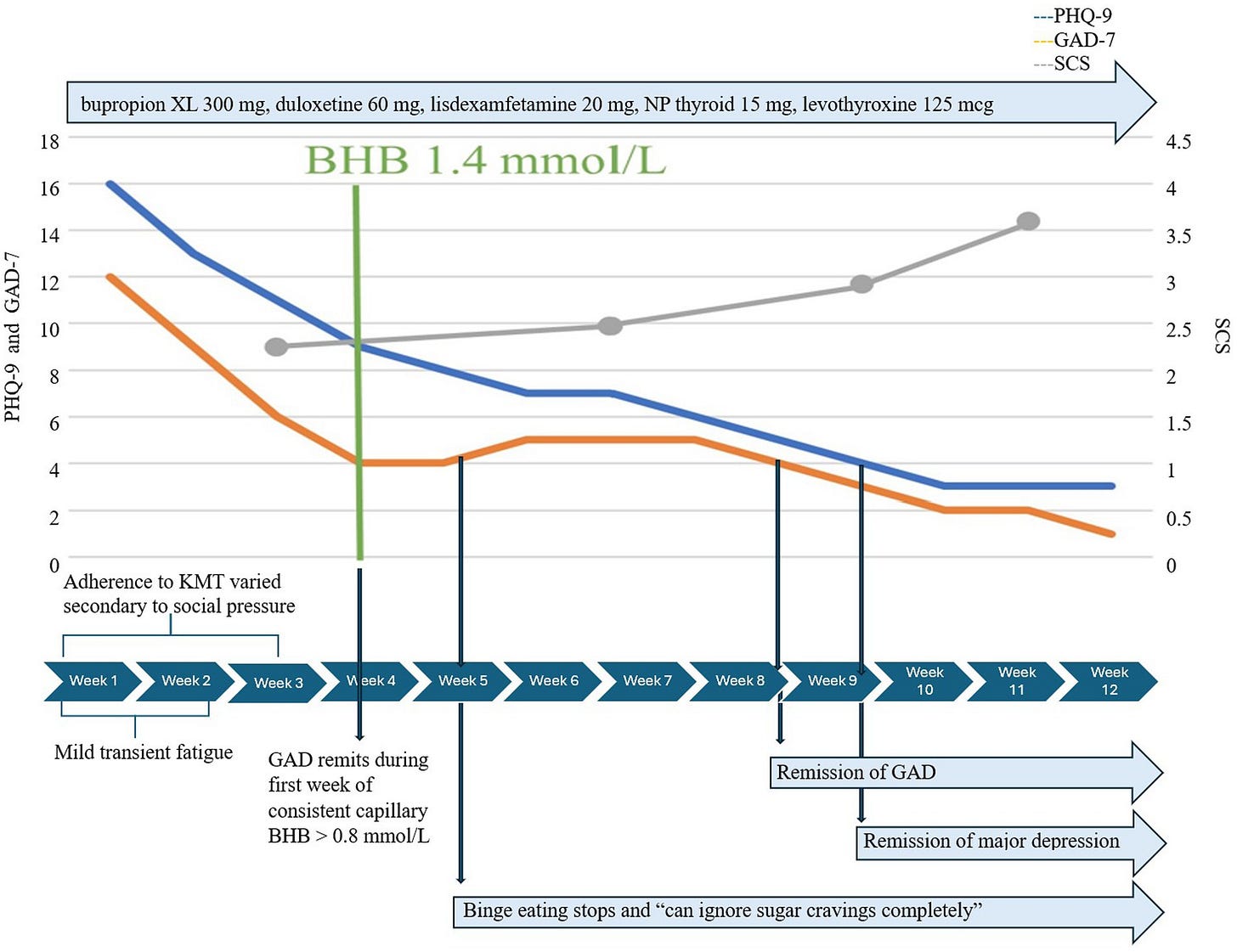
3. Complete remission of lifelong depression and anxiety with a keto diet
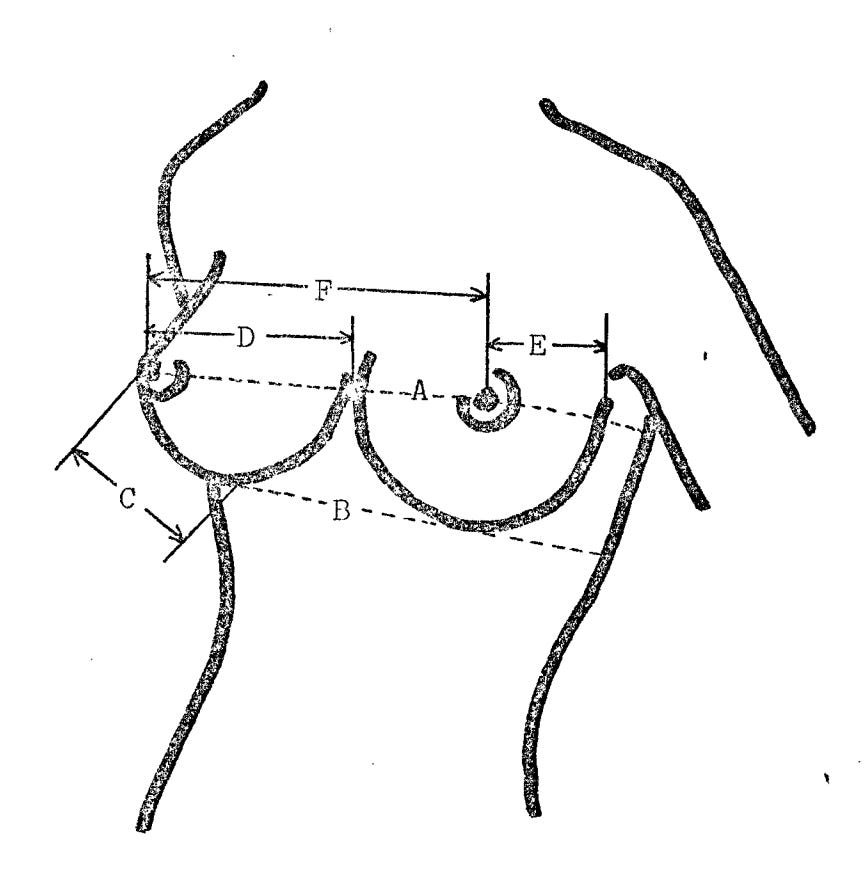
This article published just two days ago (May 14th) is about 3 case studies of 30 year olds who were able to completely resolve their depression and anxiety on a ketogenic diet. This is pretty astonishing considering one had a lifelong history of recurrent major depression, another had a lifelong history of mood dysregulation and the third had recurrent severe major depressive disorder.
The first two resolved their depression in just 7 weeks and the third took a still very short 12 weeks.
What I thought was very interesting was the authors remarking that a ketogenic diet could be effective for PTSD and obsessive doubt.
…nutritional ketosis may provide an acute and long-term intervention to reduce generalized anxiety, panic attacks, obsessive doubt, and symptoms of post-traumatic stress disorder (PTSD).
I’ve left the descriptions of each of the three people and their timeline for recovery so you can get a better idea of just how effective something as simple as the right diet change was.
Case 1 is a 32-year-old unemployed married man. He had a lifelong history of previously unrecognized and untreated recurrent major depression, as well as GAD, obsessive-compulsive disorder, trypanophobia, and binge eating disorder. He experienced prominent inattention and distractibility since childhood; an adequate prior trial of atomoxetine 100 mg po qd for 1.5 years was somewhat effective; and lisdexamfetamine 70 mg was somewhat effective. He had long declined consideration of SRIs, SNRIs, other antidepressants, and buspirone. He was unaware of the degree to which his complex symptoms had pervasively affected his functioning and quality of life, resulting in his inability to sustain employment, financial insecurity, and adverse interpersonal relationships.
Case 2 was a 36-year-old married man with a lifelong history of mood dysregulation, irritability, and trauma from adverse childhood experiences and recent work experiences. He had a history of childhood-onset generalized anxiety, panic disorder, and PTSD, as well as recurrent major depression, which was moderately severe and persistent. His anxiety was unrecognized and untreated. Although he did not have a history of mania, hypomania, or mixed states, he had been treated throughout childhood and adolescence with sertraline 50 mg (ineffective), duloxetine 60 mg (agitation), escitalopram 20 mg (diaphoresis), lamotrigine 300 mg (poor school performance), divalproex ER 1,500 mg (tremor, sluggishness, and weight gain), oxcarbazepine 1,200 mg (fatigue), olanzapine (hunger and weight gain), methylphenidate (ineffective), amphetamine-dextroamphetamine mixed salts 20 mg, and lisdexamfetamine (tachycardia). He discontinued all psychiatric treatment at age 19, but remained symptomatic for 15 years.
Case 3 was a 34-year-old single woman with a history of childhood adversity and trauma, PTSD, childhood-onset GAD, and recurrent severe major depressive disorder. She developed anorexia in adolescence and later binge eating disorder with weight fluctuations up to 100 lbs. and reported a long history of dietary attempts at weight loss, including the use of low-carb diets. She had been previously prescribed long trials of citalopram, risperidone, and ziprasidone, all of which were ineffective. ADHD, the inattentive subtype, was treated with a long-acting methylphenidate with intermittent compliance.
4. Research (yet again) finds higher cholesterol tracks with longer life
Back in a WIL Weekly from February, one of the points was “Research (again) finds higher cholesterol tracks with longer life.” Here we are again, because another March 2024 study in Cardiovascular Medicine found that having higher than recommended LDL “bad” cholesterol made people live longer:
Among primary prevention-type patients aged 50–89 years without diabetes and not on statin therapy, the lowest risk for long-term mortality appears to exist in the wide LDL-C range of 100–189 mg/dL, which is much higher than current recommendations.
5. Using vegetable oil instead of animal fat is associated with frailty
A study published just this week (May 2024) concluded that
The utilization of animal fat oil in cooking exhibited a reduced frailty risk among older adults. Conversely, transitioning from animal fat oil to vegetable oil may elevate the risk. These findings propose that substituting vegetable oil with animal fat oil in the diet may safeguard against frailty.














Does the hypnosis work on... other things....
"This is pretty astonishing"
Is it really? Curing depression is a common theme in the carnivore community, including the Peterson family. I'm not surprised keto is enough for some people. Though the paper also specifically mentions "animal-based".
Am I just in a bubble too much?